My eye-opening day in a very busy A&E department

 BBC
BBCIt’s Thursday morning at Morriston Hospital in Swansea and both staff and patients are facing a grim day.
Eight ambulances are waiting in a queue outside, 85 patients are waiting for a bed and one patient has been sitting on a hard plastic chair for 44 hours.
We are here to see the inner workings of the hospital, how the staff are working tirelessly to keep the systems running and what impact it is having on patients.
We meet some of the patients who have spent days in a hospital’s busy, noisy, windowless emergency department, where bright lights are on 24 hours a day.
They include Simon Morris, who has been on a trolley for four days due to cellulitis in his legs.
Also here is Natalie Lamb, who has been on a trolley since Monday while being treated for a blood clot.
Meanwhile, one of the senior nurses we spoke to admitted she is no longer able to provide the basics of care to all patients, saying the situation is distressing for staff.
Another staff member tells us the challenge seems insurmountable.
Upon arriving at the hospital we are given our face masks and led through a never-ending rabbit warren of corridors until we reach a small room that essentially acts as the control center for the hospital. Kind of taken down.
The meeting begins at 09:00 (GMT) and about 20 staff members briefly outline the particular challenges facing their department that day – the number of patients waiting for beds, staff illness and the number of patients being treated. Any interruptions in discharge that are fair enough, all to go home.
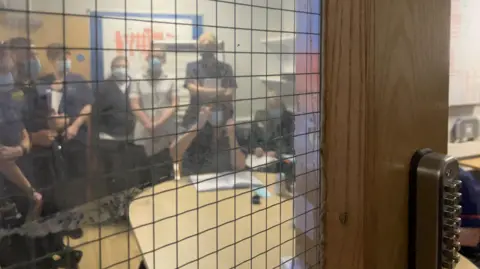
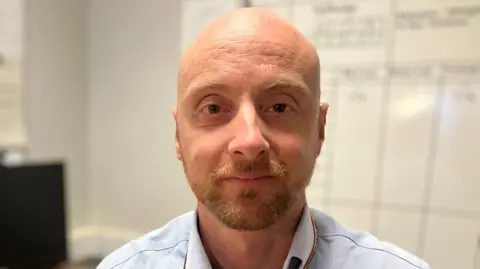
The meeting is chaired by Callum Allan-Ridge, Head of Patient Flow.
“You’re constantly trying to assess what’s going on, but you’re also predicting other sides of the puzzle where you can’t really see yet what’s going on,” says Callum.
“It’s a bit like trying to solve a Rubik’s Cube that’s trying to fight against you.”
During the meeting we learned that a patient had been waiting on a trolley in the emergency department for 139 hours, or more than five and a half days.
Another patient is well enough to go home but he can’t because he doesn’t have the house keys.
Callum admits that sometimes coming to work in the morning felt difficult.
“The task may seem insurmountable,” he says.
After the morning meeting a video call meeting is held with other hospitals in the Swansea Bay University Health Board before giving us the opportunity to meet more staff.
Consultant geriatrician Rhodri Edwards describes the pressure on the hospital as “atrocious”.
“I think the staff are very stressed, I think they feel quite demotivated and I think doctors, nurses, pharmacists and therapists may be facing burnout because of the pressures of doing their jobs.” ,
“I think everyone is very committed and really working hard to deliver the best outcomes for patients, but I think they’re really struggling with some of the challenges they’re facing, particularly Working in crowded areas, caring for patients in really busy departments.”
Dr. Edwards, who is one of the associate medical directors for acute and scheduled care, says treating patients in inappropriate areas sometimes creates privacy and dignity issues.
“People are being asked to do things they don’t feel particularly comfortable with… I think it causes an enormous amount of stress and moral injury to some employees,” he says.

Outside the hospital’s A&E entrance, ambulance paramedic Chloe Lansey is feeling dejected.
She says that just last week she brought a patient to the hospital by ambulance, left them waiting in the ambulance at the end of her shift and when she returned the next day they were still there.
“It’s terrible, it’s sad,” she says.
“This is not the job we signed up to do. We’re supposed to be out there helping people and we can’t reach them because we’re here.”
In the afternoon we are taken to the emergency department of the hospital.
As a spectator, being in a crowded, windowless space is anxiety-inducing.
Some patients are lined up on beds, others are sitting on plastic chairs and staff are stationed all around.
“It’s a noisy and busy environment, where there are no windows and where the lights are never off,” says Callum.
“For patients who are significantly unwell, it is very easy to become disoriented in the emergency department, which complicates their recovery and the outcome of their care.”
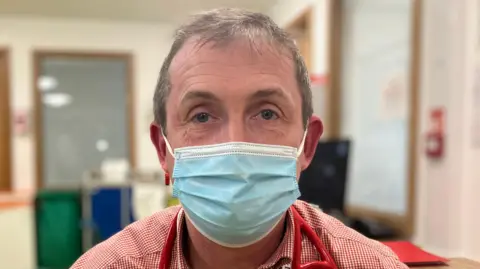
Tristan Taylor, the department’s senior charge nurse, admits, “It bothers us. I didn’t come into nursing to give this kind of standard care.”
Looking around the place, he says: “Unfortunately when you haven’t got flow in the hospital – that’s what we end up with.
“I can’t provide the basics of care to all patients – because we physically can’t do it.
“We do our best for the patient, but obviously the best is not good enough.”

Natalie Lamb was sent to A&E by her GP after experiencing shortness of breath.
After waiting for two hours in a chair in the waiting room to be told she had a blood clot in her body, she had to spend the night before being taken on a trolley to the emergency department, where she is spending her third day .
She has great sympathy and admiration for the staff and has witnessed frustrated patients yell at them.
“They get nervous trying to see everyone, they get very tired and they don’t have room to accommodate anyone,” she says.
“Something needs to be done about it.”
His colleague Karen Davis says politicians need to understand the situation better.
“It’s eye-opening, it’s disgusting,” she says.

Simon Morris has been on a trolley in a busy emergency department for four days after being brought in by ambulance with cellulitis in both legs.
He says he’s grateful to have relocated from the corridor to the bay.
“I’d rather be stuck here than stuck in the aisle, because there’s a lot of people bumping into you in the aisle, bumping into you, and they all apologize,” he says.
“The staff have been fantastic to me… I’ve seen doctors and nurses running around left, right and centre.”

The hospital is making efforts to overcome the problems
- virtual ward: Health boards say by making a patient’s home bed part of a “virtual ward” they can still offer hands-on care with the involvement of a multidisciplinary team, while avoiding avoidable hospital admissions. Can reduce and prevent the risk of hospital infections.
- Discharge of centralized hub: Launched in July 2024, a dedicated team works with third sector, local authorities and health board services to solve barriers that delay patients’ discharge. The team deals with around 20 referrals a day.
- Same day emergency care unit: this service allows patients to be assessed, diagnosed and treated on the same day they arrive at hospital after being referred by their GP, reducing the number of patients attending the emergency department Is.
- Ambulance pod: A pod outside a hospital emergency department that provides a safe and comfortable environment for patients who would otherwise be cared for in the back of an ambulance.

What is the cause of the problem? Analysis by health correspondent Owen Clark
Although I have visited many A&Es over the years – the scenes we saw in Morriston were some of the most amazing I have ever seen.
Staff are very concerned about treating patients in open spaces – it is not respectful and involves many risks.
But when so many ambulances carrying patients are stuck outside, unable to respond to emergencies, you can see why they’re using every inch of capacity.
We clearly saw a system that is struggling to cope with the enormous and growing health demands of an older as well as relatively sick and poor population.
At one level it’s a simple equation – A&E becomes overcrowded when more people come to hospital than go.
It is not surprising that efforts, where possible, are focused on preventing patients from coming to hospital or getting them out of hospital quickly.
But both small things (a patient without a key) and big things (an outbreak of infection at a nearby elderly care hospital) can hinder the work.
Families are also urged to help their loved ones get home if possible – even if it’s inconvenient – as just a little extra time off can stop a tough day from turning catastrophic.
Don’t forget too – the pressures on the NHS have been made worse by deep challenges in social care.
One A&E consultant told me that, given how many patients were coming in, it felt as if the walls of his department were made of elastic.
Some people would be surprised how far that elastic can be stretched before it breaks.
The Welsh Government urged patients to get the right care in the right place.
A spokesperson said, “Enabling people who require admission to hospital to leave hospital when they are ready is fundamentally important to improving outcomes, experiences and enabling the timely flow of patients to and from emergency departments and ambulance vehicles. Is.”
He said the Welsh Government has invested more than £180 million in extra funding this year to help manage more people safely in the community, avoid ambulance transport and hospital admissions.
Last November it launched a 50-day challenge to help speed up the hospital discharge process and he said early results had been encouraging.






