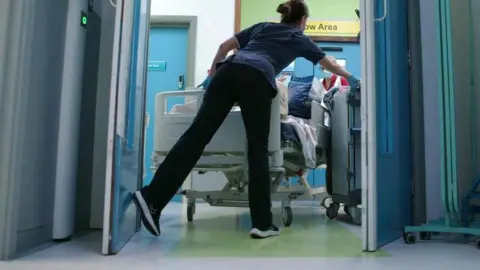
Nurses say patients are dying in hospital corridors

 getty images
getty imagesNurses say patients are dying in corridors and pregnant women are having abortions in side rooms as overcrowded hospitals struggle to cope.
The Royal College of Nursing (RCN) said evidence provided by more than 5,000 of its members across the UK this winter also showed that cupboards, car parks, bathrooms and nursing stations were being turned into temporary areas for patients. being given.
Nurses warned that such practices put patients at risk because staff were unable to access vital equipment such as oxygen, heart monitors and suction equipment, and did not have the time and space to provide CPR.
Health Secretary Wes Streeting said he agreed the problems should not be tolerated, but placed blame on the previous government.
However, RCN general secretary Professor Nicola Ranger said the findings should act as a “wake up call” for Labour.
“Patients are being stripped of their dignity and their lives are being put at risk,” he said.
Ashamed
Professor Ranger said increased investment was needed and “questions need to be asked” about whether this government has done enough to deal with the pressures seen over the winter.
More than 20 NHS trusts declared serious incidents last week, as high levels of flu and bad weather put huge pressure on hospitals.
Professor Ranger said corridor care, as it has become known, is becoming commonplace across the UK and he warned that without action it would derail the Government’s key priority of reducing waiting lists for non-urgent care in England. Will create obstacles.
RCN published more than 400 pages of testimony Asked your members about the problems they were seeing.
These include:
- People who suffer cardiac arrest remain in corridors or chambers blocked by patients on trolleys, delaying life-saving CPR.
- Others are dying on trolleys and chairs in waiting rooms and one nurse saying the NHS is “no better” than the developing world
- Women having abortions in adjacent rooms, which nurses say was not only troublesome for patients, but also made it difficult to monitor the situation.
- An incontinent, frail patient suffering from dementia having to change clothes next to a vending machine in the corridor
- Cases where 20 to 30 patients have been left in corridors under the care of one nurse and health care assistant
- Elderly patients had to sit on chairs for days and spend hours on beds in corridors in dirty clothes
“Now we have permanent corridor care,” said one nurse. “Patients don’t get the respect and care they should. Frankly, it breaks my heart.”
Another nurse, who normally works in critical care but was redeployed to A&E, said: “I felt embarrassed to work for the NHS and for the first time, I saw that it was broken. Had happened.
“I never thought in my 30-year career that this would become a ‘norm’ but it has.”
deplorable
An RCN member from the south-east of England said she is now working on the corridors almost every shift and has seen some particularly “disturbing” cases recently.
He told how a dying patient in his 90s, who had dementia and respiratory problems, was left in the corridor for eight hours and staff were unable to provide him with proper end-of-life care.
“The patient behind him was detoxing – he was vomiting and he was extremely abused. It’s not dignified. You take your dog to the vet and they’ll get better care.
“We’re not taking care of patients the way we want to.”
In a statement to the House of Commons on Wednesday about the pressures being seen this winter, Streeting blamed the previous government.
“I want to make it clear that I will never accept or tolerate the treatment of patients in corridors.
“This is unsafe, indecent, a cruel result of 14 years of failure on the NHS and I am determined to put it in the history books.
“I cannot and will not promise that there will be no more patients being treated in corridors next year, it will take time to repair the damage that has been done to our NHS.
“But that is the ambition of this government.”
Duncan Burton, chief nursing officer for NHS England, said “increasing demand” has put immense pressure on the health service in recent months, and described this winter as “one of the toughest winters the NHS has experienced”. Is.
“The impact this has on the experiences of patients and staff, as highlighted in the RCN report, should never be considered the standard to which the NHS aspires.”
Chris McCann, of patient watchdog Healthwatch England, said: “These devastating stories shared by nurses mirror the experiences people tell us about.
“Patients say they are seeing stressed and overworked staff who are bravely trying to cope with these extreme pressures.”





