‘I feel blessed to have a weight loss drug’ – but can the NHS afford it for everyone?

 BBC
BBCRay, 62, from south London, became one of the first patients to receive weight loss drug Wegovi on the NHS last year and has lost 14kg (just over two stone) in five months.
BBC Panorama joined him as he received his first dose at Guy’s Hospital in London, where he was told he would likely need to take the drug for the rest of his life to prevent weight gain. He said he felt “blessed” to be given the medicine.
But NICE, the NHS spending watchdog, has ruled that each patient can only receive Wegovi for two years. And only a tiny fraction of the 3.4 million eligible patients in England are getting the drugs.
Professor Navid Sattar, who leads the UK government Obesity Health Care Target Programsays that if everyone eligible was given the drug immediately “it would simply bankrupt the NHS”.
Being overweight is now common and almost one in three adults in England is obese – double the number of 30 years ago.
Obesity can be very bad for your health, and treating its complications is estimated to cost the NHS across the UK more than £11 billion a year.
According to trials, Vegovy and another drug called Monjaro can help patients lose about 15 to 20% of their body weight.
This type of weight loss can have dramatic effects on health, and significantly reduce a patient’s risk of many conditions from diabetes to cancer, joint problems, and heart disease.
BBC Panorama has been granted exclusive access to the weight management service at Guy’s Hospital in London, which has started rolling out Wegovi to a small group of patients who meet the criteria for body mass index (BMI).bmi) over 35 and at least one weight-related health complication.

These include care home worker Ray, who weighed 148kg or 23 stone when he started taking Wegovi in July 2024. He has struggled with his weight throughout his life.
Ray needs two operations, but doctors say he needs to lose weight first.
With so many patients meeting the criteria, the hospital is prioritizing those like Ray who need surgery or have multiple weight-related health complications.
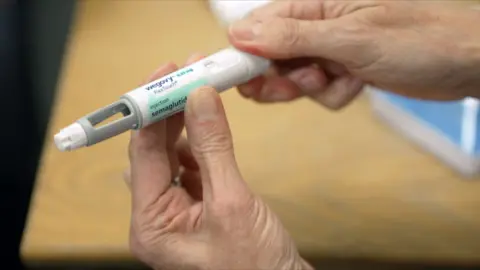
Here, not only is Ray given the medication, which is taken via weekly injections under the skin, but he also gets face-to-face support from doctors and dietitians – advice not always given to those who buy the drug privately online. She goes.
They emphasize that the vaccine does not do all the work and that it is important that patients change their lifestyle, and eat healthy food and smaller portions.
Ray was also joined at the appointment by one of his daughters, Sophie, who says it would be “amazing” if he could reach his target of losing three stone: “I wouldn’t recognize him. It would be like I had a brand new Yes, Papa.”
Right now, this medicine is available on the NHS in England through these specialist services, mostly in hospitals.
But the chances of getting medicine are less.
Of the more than 130,000 patients eligible for weight-loss drugs in south-east London, Guy’s Clinic believes it can only see around 3,000.
The weight loss drug that most people know is Ozempic. It has been in huge demand and has been popularized by celebrities from Elon Musk to Sharon Osbourne. In fact, it is for type 2 diabetes.
Wegovi contains the same ingredient, semaglutide, but in different doses.
Semaglutide mimics a gut hormone that sends signals to our brain that we are full. It also slows the transit of food through the stomach.
In trials, Wegovi reduced patients’ body weight by an average of 15% when combined with lifestyle and dietary advice.
Experts warn that the drugs should only be taken under proper medical supervision because, like all medicines, they come with side effects that not all patients can cope with.
These are mostly gastro-intestinal related – such as nausea, vomiting, diarrhea or constipation – but potentially serious complications also occur, including inflammation of the pancreas.
To help manage side effects, patients are started on a low dose of weight loss supplements and gradually increased over the course of a month.
Ray is doing well on the medication, eating smaller portions, and after five months there is a visible difference.
At the time of his appointment at Guy’s just before Christmas he weighed 134 kilograms, a weight loss of 14 kilograms or just over two stone.
He is happy. “I can’t believe how much weight I’ve lost. Whenever my daughters see me they say I’m losing weight. It’s really been a great journey.”
Ray says he feels “lucky” to have access to the medication through the NHS, especially now he is Willow’s grandfather.
Ray says that despite making several new holes in his belt, his trousers are so loose that they are falling off him.
Professor Barbara McGowan, an expert in obesity and diabetes who runs the weight management service at Guy’s, is pleased with the progress of patients like Ray.
She says most clinicians hope NICE’s two-year limit will be removed “because obesity is a chronic disease and we need to manage it long-term”.

This is no longer such an issue as a second, even more effective drug has been approved by NICE (National Institute for Health and Care Excellence).
Monjaro has been dubbed the “King Kong” of weight-loss jabs because in a major trial, patients lost an average of 21% weight over eight months.
Unlike Wegovi, there are no restrictions placed on how long NHS patients can stay on the drug.
But the NHS is set to introduce the drug in 12 years because of concerns it could impact services.
It is estimated that only 220,000 of the 3.4 million people eligible in England will benefit over the next three years.
Professor Sattar, of the University of Glasgow, says it is a simple matter of economics: “The cost of medicines is still at a level where we cannot treat several million people within the UK with these medicines. This directly impacts the NHS. Will bankrupt.
They estimate that it costs the NHS about £3,000 a year to give Monjaro or Wegovi to a patient.
So if everyone eligible in England got the drug now, it would cost around £10 billion a year – half the entire NHS medicines budget.
Jean, who is 62, hopes Monjaro will help her get her weight and health back on track. She shows me a photo of herself on her phone from a decade ago, when she looked much lighter and healthier.
“I was a die-hard fan of fitness. I went to the gym almost every day. I don’t know what happened, why I fell off the wagon.”
He believes his relationship with food is “terrible”. “I get very fussy about food and I work on it,” she says, using a term she coined to describe food cravings and preoccupation.

Jean is eligible for Monjaro because she has type 2 diabetes and has been injecting insulin for five years.
She is concerned about the side effects, which are similar to Vegovy, but will be carefully monitored at a diabetes clinic linked to Guy’s in south London.
Moonjaro helps to stabilize blood-sugar levels and promote the body’s natural production of insulin.
After only five weeks of the drug, Jean is able to stop her insulin. She’s happy: “I think it’s Monjaro, and also the willpower – I have to give myself some credit. I find the drug quiets the food noise and I don’t constantly sit around wondering what I’m going to eat. I am.”
After two months on the drug, Jean is back in the gym, and has lost over 3 kilos (half a stone).
She is disappointed with her weight loss, but is determined to lose more weight as her Monjaro dosage has been increased.
But Jean and other patients receiving Wegovi and Monjaro on the NHS are a minority.
Professor Sattar believes that nine out of 10 patients in the UK currently relying on weight loss drugs are paying for them privately.
He explains that obesity rates are highest in areas of social deprivation.
“Probably the people who are going to benefit most, who are less affluent and from more disadvantaged communities, are not going to be able to afford this drug. That’s not fair. That’s just the reality of the economics of the situation.”
But Professor Sattar told me that rising levels of obesity could eventually “bankrupt” the NHS.

With smoking levels continuing to decline, he now considers overweight and obesity to be “the major driver of many long-term health conditions, bar none.”
Both he and Professor McGowan believe weight-loss jabs have an important role to play and could ultimately lead to some widespread savings.
Professor McGowan says Ray is a good example: “We treat many of the complications associated with obesity. Ray has pre-diabetes. We are hopeful that he will recover and so will all the complications associated with that progressive disease. Will stop.
“They may require joint surgery but weight loss can prevent many complications and ultimately save the NHS a lot of money.”
Professor Sattar says that in 10 years, 20 weight loss medicines may come in the market, including some in tablet form. He says that as more effective and cheaper medicines become available, they could generate savings for the NHS.
The UK government also thinks that weight loss drugs could ultimately bring broader economic benefits.
The five-year trial in Manchester will look at the wider impact of Monjaro beyond individual health benefits, including whether it helps some people struggling with obesity get back to work.
Medicines for obesity are no magic pill, but after decades of expanding waistlines, they offer hope to millions of people.
However, right now, healthcare does not have the resources to treat all those eligible. This means – for years to come – only minorities like Ray will have access to the NHS. The rest will have to pay – or go without it.






